Recognizing the Signs and Finding Relief for a Broken Toe

A broken toe can happen to anyone, whether it is from a sudden accident or a simple misstep. The first step in treating a broken toe is recognizing the signs. Pain, swelling, bruising, and difficulty in moving the toe are common indicators. If you suspect a break, it is essential to seek medical attention promptly. To confirm the broken toe, a diagnosis is often needed by having an X-ray taken. In the meantime, you can take some steps to alleviate discomfort. Resting the affected foot and elevating it may help to reduce swelling. Immobilize the toe by buddy-taping it to an adjacent healthy toe, which can provide support and stability during the healing process. Taking over-the-counter pain relievers can help to manage pain, and it is helpful to avoid putting weight on the injured toe. If the fracture is severe or displaced, the toe may need to be reset or placed in a splint. Healing a broken toe takes time, so it is advised to be patient and take good care of your injured toe. If you have broken your toe, it is suggested that you visit a podiatrist who can effectively diagnose and treat this injury.
Broken toes may cause a lot of pain and should be treated as soon as possible. If you have any concerns about your feet, contact Dr. Odin De Los Reyes from Connecticut. Our doctor will treat your foot and ankle needs.
What Is a Broken Toe?
A broken toe occurs when one or more of the toe bones of the foot are broken after an injury. Injuries such as stubbing your toe or dropping a heavy object on it may cause a toe fracture.
Symptoms of a Broken Toe
- Swelling
- Pain (with/without wearing shoes)
- Stiffness
- Nail Injury
Although the injured toe should be monitored daily, it is especially important to have a podiatrist look at your toe if you have severe symptoms. Some of these symptoms include worsening or new pain that is not relieved with medication, sores, redness, or open wounds near the toe.
If you have any questions, please feel free to contact our offices located in Southbury and Farmington, CT . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What to Know About a Broken Toe
The forefoot is composed of five metatarsal bones and fourteen phalanges. Each toe has three phalanges except for the big toe which only has two. Our toes play an essential role to the walking process, which is why a broken toe could seriously disrupt one’s ability to move around. Toe fractures are common and can be very painful. Fortunately, these injuries rarely require surgery and usually heal with rest and a change in activity.
Broken toes typically result from a traumatic event such as falling, stubbing the toe, or dropping something on the toe. Traumatic toe fractures may be categorized as either minor or severe fractures. At times, one may hear a “pop” or “crack” sound when the bone breaks. Common symptoms of a traumatic toe fracture include pain, throbbing, bruising, swelling, and redness.
Another type of toe fractures is a stress fracture. These injuries usually appear in the form of small hairline breaks on the bone. Stress fractures develop after repetitive activity instead of a single injury. Stress fractures occur when the muscles in the bone become too weak to absorb impact. Consequently, the toe bone becomes vulnerable to any pressure and impact it endures. Symptoms for a stress fracture in the toe include swelling without bruising, tenderness to the touch, pain that goes away with rest, and pain after walking or running.
If you suspect that you have a broken toe, you should make an appointment with your podiatrist. He or she will likely diagnose you by performing a physical exam and an X-ray. Treatment for a broken toe may include the R.I.C.E. method, buddy taping, surgery, or antibiotics. The R.I.C.E. method (Rest, Ice, Compression, and Elevation) is a common treatment method for many injuries because it decreases pain. Buddy tapping involves wrapping the injured toe next to an adjacent toe to keep it supported and protected. These two methods have proven to be effective in the healing process for toe fractures. The estimated healing time for a broken toe is approximately four to six weeks. If the injury becomes infected or requires surgery, the estimated healing time may take eight weeks or more.
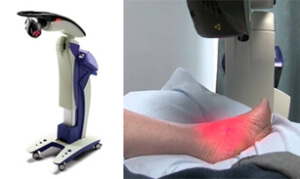
What is MLS Laser Therapy?
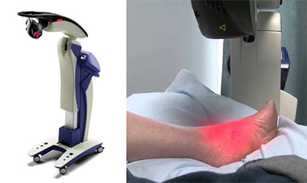 Multiwave Locked System (MLS) Laser Therapy is a laser treatment that uses a combination of wavelengths of light to reduce pain, swelling and inflammation in various parts of the body. MLS Laser Therapy can be used to treat many conditions, including arthritis and arthritic joint pain, Achilles tendon injuries, plantar fasciitis, fractures, gout, and peripheral neuropathy. MLS Laser Therapy treatment is safe, painless, and noninvasive. For some conditions, it may be used as an alternative to prescription medications and surgeries. If you are interested in exploring MLS Laser Therapy as a potential treatment option, please consult with your podiatrist.
Multiwave Locked System (MLS) Laser Therapy is a laser treatment that uses a combination of wavelengths of light to reduce pain, swelling and inflammation in various parts of the body. MLS Laser Therapy can be used to treat many conditions, including arthritis and arthritic joint pain, Achilles tendon injuries, plantar fasciitis, fractures, gout, and peripheral neuropathy. MLS Laser Therapy treatment is safe, painless, and noninvasive. For some conditions, it may be used as an alternative to prescription medications and surgeries. If you are interested in exploring MLS Laser Therapy as a potential treatment option, please consult with your podiatrist.
MLS Laser Therapy is a successful alternative for treating any pain you may be experiencing related to certain podiatric conditions. If you are interested in MLS Laser Therapy, consult with Dr. Odin De Los Reyes from Connecticut. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
MLS Laser Therapy
Multiwave Locked System (MLS) Laser Therapy is a patented, FDA-cleared technology that helps relieve pain and inflammation from a number of podiatric conditions, including:
- Heel Pain
- Plantar Fasciitis
- Sports Injuries
- Wounds
- Achilles Tendonitis
- Arthritis
- Neuropathy
- Neuromas
MLS Laser Therapy is an ideal alternative to surgery and prescription medication, as it has no negative side effects and encourages accelerated healing. Among its many clinical benefits, MLS Laser Therapy also:
- Reduces swelling due to bruising or inflammation
- Blocks pain
- Reduces formation of scar tissue
- Improves nerve function
If you have any questions, please feel free to contact our offices located in Southbury and Farmington, CT . We offer the newest diagnostic and treatment technologies for all your foot care needs.
MLS Laser Therapy
MLS Laser Therapy is an FDA-approved technology designed to treat various painful conditions. It is often sought out as a successful alternative to surgical treatment and prescription medication that may otherwise bring about negative side effects. During MLS Laser Therapy, light energy enters the damaged cells to stimulate intercellular activity, reducing pain in the affected area and accelerating the recovery process.
MLS Laser Therapy is used in podiatry to treat various conditions. These include heel pain, plantar fasciitis, sports injuries, wounds, Achilles tendonitis, arthritis, neuromas, neurological pain, musculoskeletal disorders, and sore muscles. Aside from the specific conditions MLS Laser Therapy treats, patients can also gain from the treatment’s general benefits. These benefits include a rapid relief of pain, the reduction of swelling caused by inflammation or bruising, faster healing, improved blood circulation, the reduction of scar tissue, and improved nerve function.
MLS Laser Therapy is a non-surgical treatment with no side effects. The treatment process is painless and typically takes a short amount of time to complete. Several treatments may be required depending on the specific condition.
Heel Pain and Obesity

Heel pain is a common complaint that can affect anyone, but it can be particularly challenging for those who are obese. The excess weight places additional stress on the feet, especially the heels, which bear the brunt of the load. This extra pressure can lead to various painful conditions, including plantar fasciitis, heel spurs, and Achilles tendonitis. Plantar fasciitis, in particular, is a frequent cause of heel pain. The plantar fascia, a thick band of tissue that runs along the bottom of the foot, can become strained and inflamed due to the increased weight. Fortunately, there are ways to manage and alleviate heel pain in obese individuals. Weight loss can significantly reduce the pressure on the feet and the pain. Wearing supportive footwear, custom orthotics, and stretching exercises may also help relieve discomfort. It is essential for those struggling with obesity to address their heel pain, as it can hinder mobility and overall well-being. Seeking help from a podiatrist is a crucial step toward finding relief and improving foot health. If you have heel pain and are overweight, it is suggested that you speak with this type of healthcare professional who can help you manage both conditions.
Obesity has become very problematic at this point in time and can have extremely negative effects on the feet. If you’re an obese individual and are concerned about your feet, contact Dr. Odin De Los Reyes from Connecticut. Our doctor can provide the care you need to keep you pain-free and on your feet.
Obesity and Your Feet
Since your feet are what support your entire weight when standing, any additional weight can result in pain and swelling. Being overweight is one of the main contributors to foot complications.
Problems & Complications
Extra Weight – Even putting on just a few extra pounds could create serious complications for your feet. As your weight increases, your balance and body will shift, creating new stresses on your feet. This uneven weight distribution can cause pain, even while doing the simplest tasks, such as walking.
Diabetes – People who are overweight are at serious risk of developing type-2 diabetes, which has a drastic impact on the health of your feet. As you get older, your diabetes might worsen, which could lead to loss of feeling in your feet, sores, and bruises. You could also become more prone to various infections.
Plantar fasciitis – Pressure and stress that is placed on muscles, joints, and tendons can trigger plantar fasciitis, which is an inflammation of tissue that forms along the bottom of the foot.
If you have any questions please feel free to contact our offices located in Southbury and Farmington, CT . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
How Obesity Affects Your Feet
Gaining weight can happen suddenly and at any time. Usually you won’t notice the extra weight until your feet start hurting at the end of the day. This happens as your feet begin adjusting to carrying more weight. Foot swelling and pain are two of the biggest side effects of having gained weight.
Many foot-related problems can occur even after just putting on a few pounds. This includes the body ‘compensating’ by changing the way it moves. You may find yourself putting extra weight on the wrong parts of your feet and even leaning forward a bit. Your feet were designed to carry a healthy, normal body weight. Extra weight places undue stress on them.
Being overweight often causes the development of Type-2 diabetes, causing leg and foot pain. Older people who do not attempt to control their condition can even lose sensation and feeling in their legs and feet. This can lead to the development of small sores that can lead to serious infection.
Extra stress placed on the joints, tendons and muscles in the feet as a result of extra body weight may also cause heel spurs, or plantar fasciitis. Plantar fasciitis is an inflammation of the foot tissue, causing stiffness and pain when walking and climbing stairs. This can usually be relieved by foot stretches and custom made orthotic shoe-inserts.
Problems in the feet triggered by obesity can be treated by paying special attention to footwear. Proper support shoes that allow for good circulation, especially in the arch and ankle, are vital. A podiatrist can help you find what sort of shoe is most suitable for your feet. They can also measure you for special orthotics if necessary.
It could also be high time to start losing weight in order to treat and prevent diabetes as well as other life threatening diseases. Some methods include yoga and water aerobics, which benefit your entire body without placing stress on your feet. Don’t risk losing your feet by losing interest in them. Take care of your feet and your body, as they deserve the very best.
Causes Symptoms and Treatment for Poor Circulation in the Feet
The purpose of the body’s circulation system is to transport blood, oxygen, and nutrients throughout the body. A reduction of blood to a specific part of the body may cause one to experience symptoms of poor circulation. The most common causes of poor circulation in the feet are obesity, diabetes, and heart conditions such as peripheral artery disease (PAD). Common symptoms of poor circulation include tingling, numbness, throbbing, pain and muscle cramps.
Peripheral artery disease is a common cause of poor circulation in the legs. Symptoms of PAD are cramping, pain or tiredness in the leg or hip muscles while walking or climbing stairs. This pain tends to go away with rest and starts back up when you begin to walk. It is a condition that causes the blood vessels and arteries to become narrow. Although PAD is more common in adults over the age of 50, it may also occur in younger people. A similar condition called atherosclerosis causes arteries to stiffen up due to a buildup of plaque in the arteries and blood vessels.
Blood clots are also a common cause of poor circulation in the feet. Clots may obstruct blood vessels and if they occur in the legs, they may eventually lead to pain and discoloration. This occurrence is commonly known as deep vein thrombosis (DVT) and it may travel to the lungs. Varicose veins are another condition that may lead to poor circulation, and it is caused by incompetence of the valves in the veins. Women who are overweight are prone to developing this condition. Lastly, diabetes, which is correlated with poor blood sugar metabolism may lead to chronic poor circulation. Those with diabetes often suffer from cramping in the legs, calves, thighs and buttocks.
If you are looking for ways to avoid poor circulation there are some tips you can follow. One tip is to avoid sitting for too long. If you plan to sit down for a long period of time, you should try standing up occasionally, to improve your circulation. Another great way to avoid poor circulation is to exercise. Exercise is an excellent way to pump the heart and increase blood flow. Those who suffer from poor circulation should also avoid smoking, reduce their salt intake, and try to lose weight.
If you are experiencing symptoms from poor circulation in your feet, you should consult with your podiatrist to determine the best method for treatment for you. He or she may prescribe medication in addition to recommending specific lifestyle changes to improve your circulation.
Causes and Treatment for Sever’s Disease
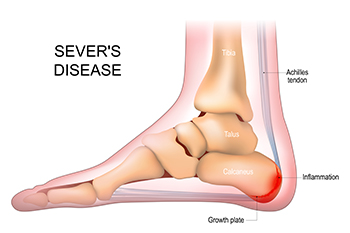
Sever's disease, which is also known as calcaneal apophysitis, is a common ailment affecting young athletes. This condition arises during the child's growth spurt years when the heel bone's growth plate becomes inflamed as a result of repetitive stress. Sporting activities involving running and jumping can exacerbate the condition. The intensity of physical activity, coupled with the bones growing at different rates, puts strain on the developing heel. The result is pain and tenderness that can disrupt a young athlete's active life. Thankfully, effective treatments exist. Rest and activity modification can help to alleviate pressure, in addition to elevating the affected foot. Performing stretching exercises that target calf muscles and wearing supportive, cushioned footwear also can aid in recovery. Consulting a podiatrist is important for an accurate diagnosis and a tailored treatment plan. With appropriate care, Sever's disease can be managed, ensuring a smoother journey toward adulthood's peak physical performance. If your child has heel pain, it is suggested that you consult this type of doctor who can treat Sever’s disease.
Sever's disease often occurs in children and teens. If your child is experiencing foot or ankle pain, see Dr. Odin De Los Reyes from Connecticut. Our doctor can treat your child’s foot and ankle needs.
Sever’s Disease
Sever’s disease is also known as calcaneal apophysitis, which is a medical condition that causes heel pain I none or both feet. The disease is known to affect children between the ages of 8 and 14.
Sever’s disease occurs when part of the child’s heel known as the growth plate (calcaneal epiphysis) is attached to the Achilles tendon. This area can suffer injury when the muscles and tendons of the growing foot do not keep pace with bone growth. Therefore, the constant pain which one experiences at the back of the heel will make the child unable to put any weight on the heel. The child is then forced to walk on their toes.
Symptoms
Acute pain – Pain associated with Sever’s disease is usually felt in the heel when the child engages in physical activity such as walking, jumping and or running.
Highly active – Children who are very active are among the most susceptible in experiencing Sever’s disease, because of the stress and tension placed on their feet.
If you have any questions, please feel free to contact our offices located in Southbury and Farmington, CT . We offer the newest diagnostic and treatment technologies for all your foot and ankle injuries.
Sever's Disease
Sever's disease, also known as calcaneal apophysitis, is a medical condition that causes heel pain in children’s feet while they’re growing. Sever's disease occurs most commonly in boys and girls between the ages of 8 and 14.
Sever's disease occurs when the child’s growth plate, or the calcaneal epiphysis, an area attached to the Achilles tendon, is injured or when the muscles and tendons of the growing foot do not keep pace with bone growth. The result is constant pain experienced at the back of the heel and the inability to put any weight on the heel. This forces the child to bear weight on their toes while walking. When a toe gait develops, the child must change the way they walk to avoid placing weight on the painful heel. If this is not properly addressed, this can lead to further developmental problems.
The most common symptom of Sever's disease is acute pain felt in the heel when a child engages in physical activity such as walking, jumping or running. Children who are active athletes are among the group most susceptible to experiencing Sever's disease. This is due to the extreme stress and tension placed on their growing feet. The rolling movement of the foot during walking or running and obesity are both additional conditions linked to causing Sever's disease.
The first step in treating Sever's disease is to rest the foot and leg and avoid physical activity. Over the counter pain-relieving and anti-inflammatory medications can be helpful for reducing the amount of heel pain. A child with Sever's disease should also wear shoes that properly support the heel and the arch of the foot. Consider purchasing orthotic shoe inserts which can help support the heel and foot while it is healing. Most patients with Sever's disease symptoms report an eventual elimination of heel pain after wearing orthotic insoles that support the affected heel.
Sever's disease may affect either one heel or both. It is important for a child experiencing heel pain to be examined by a foot doctor who can apply the squeeze test. The squeeze test compresses both sides of the heel in order to determine if there is intense pain. Discourage any child diagnosed with Sever's disease from going barefoot as this can intensify the problem. Apply ice packs to the affected painful heel two or three times a day for pain relief.
Exercises that help stretch the calf muscles and hamstrings are effective at treating Sever's disease. An exercise known as foot curling has also proven to be very effective at treating Sever's disease. When foot curling, the foot is pointed away from the body, then curled toward the body to help stretch the muscles. The curling exercise should be done in sets of 10 or 20 repetitions and repeated several times throughout the day.
Treatment methods can continue for at least 2 weeks and as long as 2 months before the heel pain completely disappears. A child can continue doing daily stretching exercises for the legs and feet to prevent Sever’s disease from returning.