Swelling of the Feet
There are many reasons why patients experience swelling of the feet. It is rather common and may be a side effect of pregnancy or from sitting and standing for most of the day. Gravity could also play a role in the development of swollen feet. It is known that the weight of blood volume in our bodies is exerted on the veins in the legs and feet. The veins may not work as efficiently during the aging process, and this could make the blood flow backward causing swollen feet. Relief may be found when obese patients lose weight, and it may help to engage in compression therapy by wearing compression socks, stockings, or athletic sleeves. This method can release pressure on the feet and ankles which may help to reduce existing swelling. There are patients who have controlled their swollen feet by implementing healthy lifestyle changes. These can consist of reducing salt intake, incorporating a gentle exercise regime into the daily routine, and drinking plenty of fresh water. Swollen feet may be a temporary condition that affects people who travel via airplane or automobile, so it is beneficial to walk as frequently as possible even though it can be difficult. Swelling of the feet can also be indicative of other health issues so it is important to pay attention to any type of chest pain, mental confusion, dizziness, or fever. If you consistently have swollen feet, it is strongly suggested that you consult with a podiatrist who can help determine the cause and how to effectively treat it.
Running Injuries That Affect the Feet and Ankles

Running is a fantastic way to stay fit, boost cardiovascular health, and enjoy the great outdoors. Despite its many benefits, running can also take a toll on your feet and ankles. More than 80 percent of running injuries are attributed to repetitive stress, making it important for runners to be aware of the potential pitfalls and methods to prevent and address them. The repetitive impact of every foot strike during your runs can put significant stress on your muscles, joints, and connective tissues, increasing the risk of injury. Foot injuries are a significant concern for runners. Plantar fasciitis, metatarsalgia, and stress fractures are some of the more common conditions that can affect the feet. These injuries can cause intense pain, particularly during the push off phase of running. Ankles are susceptible to sprains, strains, and ligament injuries in runners. Running on uneven terrain and wearing improper footwear can contribute to these injuries, which may result in instability and limited mobility. If you experience pain or discomfort in the feet or ankles from your running, it is suggested that you make an appointment with a podiatrist for an exam, diagnosis, and tips for preventing injuries.
All runners should take extra precaution when trying to avoid injury. If you have any concerns about your feet, contact Dr. Odin De Los Reyes of Connecticut. Our doctor will treat your foot and ankle needs.
How to Prevent Running Injuries
There are a lot of mistakes a runner can make prior to a workout that can induce injury. A lot of athletes tend to overstretch before running, instead of saving those workouts for a post-run routine. Deep lunges and hand-to-toe hamstring pulls should be performed after a workout instead of during a warmup. Another common mistake is jumping into an intense routine before your body is physically prepared for it. You should try to ease your way into long-distance running instead of forcing yourself to rush into it.
More Tips for Preventing Injury
- Incorporate Strength Training into Workouts - This will help improve the body’s overall athleticism
- Improve and Maintain Your Flexibility – Stretching everyday will help improve overall performance
- “Warm Up” Before Running and “Cool Down” Afterward – A warm up of 5-10 minutes helps get rid of lactic acid in the muscles and prevents delayed muscle soreness
- Cross-Training is Crucial
- Wear Proper Running Shoes
- Have a Formal Gait Analysis – Poor biomechanics can easily cause injury
If you have any questions, please feel free to contact our offices located in Southbury and Farmington, CT . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Preventing Running Injuries
Over half of all runners encounter at least one injury per year. The reason for this is because many runners do not train properly. Injuries are almost inevitable due to the physical stress that running causes. While our bodies are great at adapting to the stress, it can only handle it in small doses. Injuries occur when the stress is applied too quickly for the body to handle, causing something within it to break down. With each step you take, your leg is absorbing two or three times your body’s weight.
Some of the most popular running injuries are shin splints, plantar fasciitis, Achilles tendinitis, and stress fractures. Shin splints cause pain along the inside or outside of the shins, and this pain is usually felt at the beginning of a run. The condition itself is defined as an inflammation of the muscles or tendons located around the shinbone. To treat shin splints, it is advised that you ice the shin area and stretch the calf muscles. To prevent this injury, you should slowly increase the distance you plan on running, instead of jumping into a more strenuous routine.
Achilles tendinitis is another common injury and it feels like pain along the back of the leg, toward the heel. This condition is defined as an inflammation of the Achilles which is the largest tendon in the body. The Achilles is responsible for connecting your calf muscles to the heel bone and it is caused by tight calf muscles. If you want to treat this injury, you should take a break from running to cross train with a low-impact activity.
There are a lot of common mistakes runners make that are causing them to experience injury. One mistake is stretching too much prior to warming up. If you plan to go on a run, you should warm up with a gentle 3-5-minute walk followed by a 5-minute run-walk. Another common mistake is jumping into a routine too quickly. Consequently, you should incorporate cross-training into your routine. If you are looking to get active, you should slowly weave running into an activity you are currently participating in. For example, you can try bike riding for 40 minutes followed by a 10-minute run.
Another way to prevent running injuries is to choose shoes that are appropriate for running. There are certain things you should look for when buying a new pair of running shoes. An important factor in these sneakers is flexibility. Running shoes should be capable of bending and flexing at the forefoot. However, you should not be able to bend the entire shoe in half with ease because this is a sign that the shoe does not have enough structure. Additionally, you should look for the fit of the running shoes you want to purchase. It is best to visit a specialty running shoe store to have your feet properly sized. Choosing shoes that fit properly can prevent many foot ailments.
If you are suffering from any pain from running injuries, you should make an appointment with your podiatrist to discover the underlying cause of your pain. He or she will be able to help treat your condition in the best way possible.
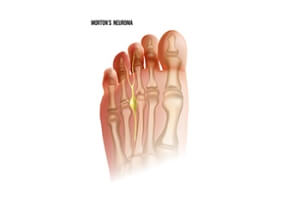
Common Symptoms of Morton's Neuroma
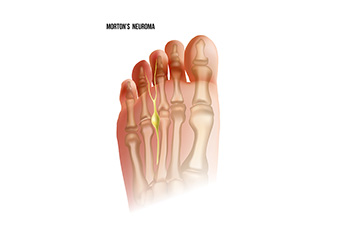
Morton's neuroma is a foot condition that often goes under the radar but can cause significant discomfort. It occurs when the tissue surrounding the nerves leading to the toes thickens, resulting in nerve compression. This compression can lead to a variety of unpleasant symptoms. Foremost is pain, typically felt in the ball of the foot or between the third and fourth toes. This pain is often described as a sharp or burning sensation, and patients may liken it to having a pebble in their shoe. Many individuals with Morton's neuroma experience tingling or numbness in the affected toes. Symptoms can worsen with activities that place pressure on the foot, such as walking or wearing tight shoes. If you are experiencing signs of Morton’s neuroma, it is suggested that you confer with a podiatrist who can properly diagnose and treat this condition.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Dr. Odin De Los Reyes of Connecticut. Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our offices located in Southbury and Farmington, CT . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Morton's Neuroma
Morton's Neuroma, also called Intermetatarsal Neuroma or Plantar Neuroma, is a condition that affects the nerves of the feet, usually the area between the third and fourth toe. Neuroma refers to a benign growth that can occur in different parts of the body. Morton's Neuroma strictly affects the feet. This condition causes the tissue around the nerves that lead to the toes becoming thick, causing pain in the ball of the foot.
This condition can be caused by injury, pressure or irritation. Normally no lump will be felt, but instead burning pain in the ball of the foot will be experienced. Numbness and tingling may also occur. With the onset of this condition, a person may feel pain when tight or narrow shoes are worn. As the condition worsens, the pain may persist for days, or even weeks.
Persistent foot pain should always be a concern. The foot should be examined by a podiatrist if pain persists longer than a few days with no relief from changing shoes. The earlier the foot is examined and treated, the less chance there will be for surgical treatment.
There are some factors that can play a role in the development of Morton's Neuroma. These include wearing ill-fitting shoes that cause pressure to the toes, such as high heels. Also, high impact exercise may contribute to the cause of this condition. Morton’s Neuroma may also develop if the foot sustains an injury. Another cause includes walking abnormally due to bunions or flat feet. This causes excessive pressure and irritates the tissue. At times, people are affected for no determinable reason.
Podiatrists can alleviate the effects of this condition using a treatment plan to help decrease the pain and heal the foot tissue. Depending upon the severity of the Morton's Neuroma, the treatment plan can vary. For cases that are mild to moderate, treatments may include applying padding to the arch to relieve pressure from the nerve and reduce compression while walking. Ice packs can also help reduce swelling. The podiatrist may also create a custom orthotic device to support the foot and reduce compression and pressure on the affected nerve. The doctor will probably advise against partaking in activities that cause constant pressure on the affected area. They may provide wider shoes to ease the pressure from the toes. If these treatments do not relieve the symptoms of this condition, the doctor may use injection therapy.
Surgical treatment may be recommended by the podiatrist if all other treatments fail to provide relief. Normally, the podiatric surgeon will decide on either a surgical procedure that involves removal of the affected nerve or will choose surgery to release the nerve. After examination, the surgeon will decide on the best approach to treat the problem.
Recovery varies according to the type of surgical procedure. The patient will also be instructed on the best shoe wear to prevent the return of this condition, along with changes to workout routines, if this was a cause. Preventative measures are important in ensuring the condition does not return.
Unveiling the Causes of Nighttime Foot Pain

Experiencing foot pain at night can be incredibly disruptive, robbing you of a restful sleep. The causes of nocturnal foot pain can be diverse and often rooted in our daily activities. One common culprit is overuse or excessive strain during the day, especially if your job demands prolonged standing or walking. Conditions like plantar fasciitis, characterized by inflammation of the tissue that connects the heel to the toes, tend to worsen during periods of inactivity and can cause discomfort at night. Additionally, flat feet or fallen arches can contribute to nighttime foot pain due to altered alignment and increased pressure on certain areas. Osteoarthritis, rheumatoid arthritis, and gout can also flare up during the night, causing pain, throbbing or aching sensations. If you experience persistent or severe foot pain at night, it is suggested that you visit a podiatrist who can determine what cause and offer effective remedies for a good night's rest.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with Dr. Odin De Los Reyes from Connecticut. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our offices located in Southbury and Farmington, CT . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot Pain
The feet, being the foundation of the body, carry all of the body’s weight and are therefore prone to experiencing pain and discomfort. If you are experiencing foot pain, it is important to determine where in the foot you are experiencing this pain to help discover the cause of it. While pain can be experienced virtually anywhere in the foot, the most common sites of foot pain are in the heel and ankle.
Heel pain can be due to a multitude of conditions including plantar fasciitis, Achilles tendinitis, and heel spurs. Pain experienced in the ankle can be a sign of an ankle sprain, arthritis, gout, ankle instability, ankle fracture, or nerve compression. In more serious cases, pain in the foot can be a sign of improper alignment or an infection.
Foot pain can be accompanied by symptoms including redness, swelling, stiffness and warmth in the affected area. Whether the pain can be described as sharp or dull depends on the foot condition behind it. It is important to visit your local podiatrist if your foot pain and its accompanying symptoms persist and do not improve over time.
Depending on the location and condition of your foot pain, your podiatrist may prescribe certain treatments. These treatments can include but are not limited to prescription or over-the-counter drugs and medications, certain therapies, cortisone injections, or surgery.
If you are experiencing persistent foot pain, it is important to consult with your foot and ankle doctor to determine the cause and location. He or she will then prescribe the best treatment for you. While milder cases of foot pain may respond well to rest and at-home treatments, more serious cases may take some time to fully recover.
Arthritis Can Cause Pain in the Feet and Ankles
Treatment for Cracked Heels

Cracked heels are a common foot condition characterized by the splitting of dry, thick skin on the heels. When only the outer layer of skin is affected, it may not be painful but can be uncomfortable. In more severe cases, the cracks can extend into the healthy skin, causing pain, bleeding, and infection risk. Several factors contribute to cracked heels, including prolonged standing, wearing unsupportive footwear, and biomechanical issues. Additionally, taking hot showers, increase in weight, and medical conditions such as diabetes may contribute to developing cracked heels. They are often more prevalent in the summer due to wearing open-back shoes and warm weather. Symptoms of cracked heels often include discomfort, pain while standing, itchiness, and dry, white skin on the heels. Treatment involves removing the dry skin, addressing underlying problems or infections, and preventing recurrence. Prevention strategies include regular callus removal, daily moisturizing, and wearing appropriate footwear. If you are suffering from cracked heels and they are not responding to everyday foot care, it is suggested that you consult a podiatrist for a specialized treatment plan.
If the skin on your feet starts to crack, you may want to see a podiatrist to find treatment. If you have any concerns, contact Dr. Odin De Los Reyes from Connecticut. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
It is important to moisturize your cracked heels in order to prevent pain, bleeding, and infection. The reason cracked heels form is because the skin on the foot is too dry to support the immense pressure placed on them. When the foot expands, the dry skin on the foot begins to split.
Ways to Help Heal Them
- Invest in a good foot cream
- Try Using Petroleum Jelly
- Ease up on Soaps
- Drink Plenty of Water
Ways to Prevent Cracked Heels
- Moisturize After Showering
- Skip a Shower
- Keep Shower Water Lukewarm
- Don’t Scrub Your Feet
If you are unsure how to proceed in treating cracked heels, seek guidance from a podiatrist. Your doctor will help you with any questions or information you may need.
If you have any questions, please feel free to contact our offices located in Southbury and Farmington, CT . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Solutions for Cracked Heels
Cracked heels can make life very frustrating and embarrassing when displaying the bare feet. Aside from being unpleasing to the eye, they can also tear stockings and socks and wear out shoes at a faster rate. When severe, cracked heels may cause pain or infection.
Cracked heels are a problem for those who are athletic, those who may walk a lot, and those who have especially dry skin. Those who use medication that dry the skin, those who swim often, wearing certain types of shoes, and those who are diabetic may have trouble with cracked heels. Seniors whose skin produces less oil may also have trouble with cracked feet. There is no one way to develop cracked feet, and there is no cure.
Today, the market consists of numerous products that have a variety of ingredients to promote healing. Some of these are over-the-counter. Others are prescribed by a doctor, especially for those who have chronic dry feet and heels.
Some doctors recommend wearing socks at night for those with rough skin. This helps further healing, and helps creams stay on longer and better absorb into the skin.
One way to alleviate dryness that causes cracked heels is by using moisturizers both day and night. Another way is to make sure the skin is clean and dry at all times. Using a pumice stone to buff away dead skin before putting on moisturizer can also help. Cracked heels will not respond to the cream unless the outer layer of skin is first removed through exfoliation. After exfoliation, lotion or ointment will be absorbed by the skin more easily.
Foods that produce healing and balance can also help the skin from within. Everything that is put into the body can either help it or hurt it. Taking supplements of omega-3 fatty acids and zinc can also be very beneficial.
Nevertheless, not all products are guaranteed to help treat cracked feet. Seeing a professional is best if other treatments options were unsuccessful. A podiatrist should be able to give the best advice to help with this problem.